Group A Streptococcal (GAS) Infections: Background, Pathophysiology, Etiology
Streptococci are a large group of gram-positive, nonmotile, non–spore-forming cocci about 0.5-1.2µm in size. They often grow in pairs or chains and are negative for oxidase and catalase.
S pyogenes tends to colonize the upper respiratory tract and is highly virulent as it overcomes the host defense system. The most common forms of S pyogenes disease include respiratory and skin infections, with different strains usually responsible for each form.
The cell wall of S pyogenes is very complex and chemically diverse. The antigenic components of the cell are the virulence factors. The extracellular components responsible for the disease process include invasins and exotoxins. The outermost capsule is composed of hyaluronic acid, which has a chemical structure resembling host connective tissue, allowing the bacterium to escape recognition by the host as an offending agent. Thus, the bacterium escapes phagocytosis by neutrophils or macrophages, allowing it to colonize. Lipoteichoic acid and M proteins located on the cell membrane traverse through the cell wall and project outside the capsule.
Mục Lục
Epithelial cell invasion
A characteristic of S pyogenes is the organism’s ability to invade epithelial cells. Failure of penicillin to eradicate S pyogenes from the throats of patients, especially those who are carriers of S pyogenes, has been increasingly reported. The results of one study strongly suggested that if the carrier state results from intraepithelial cell streptococci survival, the failure of penicillin to kill ingested S pyogenes may be related to a lack of effective penicillin entry into epithelial cells.
[7] These observations may have clinical implications for understanding carriers and managing S pyogenes infection.
Bacterial virulence factors
The cell wall antigens include capsular polysaccharide (C-substance), peptidoglycan and lipoteichoic acid (LTA), R and T proteins, and various surface proteins, including M protein, fimbrial proteins, fibronectin-binding proteins (eg, protein F), and cell-bound streptokinase.
The C-substance is composed of a branched polymer of L-rhamnose and N -acetyl-D-glucosamine. It may have a role in increased invasive capacity. The R and T proteins are used as epidemiologic markers and have no known role in virulence.
[8]
Another virulence factor, C5A peptidase, destroys the chemotactic signals by cleaving the complement component of C5A.
M protein, the major virulence factor, is a macromolecule incorporated in fimbriae present on the cell membrane projecting on the bacterial cell wall. It is the primary cause of antigenic shift and antigenic drift among GAS.
[9, 10]
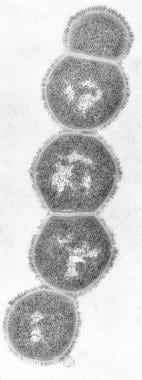
Streptococcus group A infections. M protein.
View Media Gallery
M protein binds the host fibrinogen and blocks the binding of complement to the underlying peptidoglycan. This allows survival of the organism by inhibiting phagocytosis. Strains that contain an abundance of M protein resist phagocytosis, multiply rapidly in human tissues, and initiate the disease process. After an acute infection, type-specific antibodies develop against M protein activity in some cases.
Although such antibodies protect against infection by a homologous M protein type, they confer no immunity against other M types. This observation is one of the factors representing a major theoretical obstacle to the S pyogenes vaccine design, because more than 80 M serotypes have been described to date.
Community-based outbreaks of particular streptococcal diseases tend to be associated with certain M types; therefore, M serotyping has been very valuable for epidemiologic studies.
Bacterial adherence factors
At least 11 different surface components of GAS have been suggested to play a role in adhesion. In 1997, Hasty and Courtney proposed that GAS express different arrays of adhesins in various environmental niches. Based on their review, M protein mediates adhesion to HEp-2 cells, but not to buccal cells, in humans, whereas FBP54 mediates adhesion to buccal cells, but not to HEp-2 cells. Protein F mediates adhesion to Langerhans cells, but not to keratinocytes.
One of the theories proposed with regard to the process of adhesion is a 2-step model. The initial step in overcoming the electrostatic repulsion of the bacteria from the host is mediated by LTA, which provides weak, reversible adhesion. The second step takes the form of firm, irreversible adhesion mediated by tissue-specific M protein, protein F, or FBP54, among others. Once adherence has occurred, the streptococci resist phagocytosis, proliferate, and begin to invade the local tissues.
[11]
GAS show enormous and evolving molecular diversity, driven by horizontal transmission among various strains. This is also true when they are compared with other streptococci. Acquisition of prophages accounts for much of the diversity, conferring not only virulence via phage-associated virulence factors but also increased bacterial survival against host defenses.
Extracellular products and toxins
Various extracellular growth products and toxins produced by GAS are responsible for host cell damage and inflammatory response.
Hemolysins
S pyogenes elaborates 2 distinct hemolysins. These proteins are responsible for the zone of hemolysis observed on blood agar plates and are also important in the pathogenesis of tissue damage in the infected host. Streptolysin O is toxic to a wide variety of cell types, including myocardium, and is highly immunogenic. The determination of the antibody responses to this protein (antistreptolysin O [ASO] titer) is often useful in the serodiagnosis of recent infection.
Streptolysin S is another virulence factor capable of damaging polymorphonuclear leukocytes and subcellular organelles. However, in contrast to streptolysin O, it does not appear to be immunogenic.
Pyrogenic exotoxins
The family of streptococcal pyrogenic exotoxins (SPEs) includes SPEs A, B, C, and F. These toxins are responsible for the rash of scarlet fever. Other pathogenic effects caused by these substances include pyrogenicity, cytotoxicity, and enhancement of susceptibility to endotoxin. SPE B is a precursor of a cysteine protease, another determinant of virulence.
[12]
Group A streptococcal isolates associated with streptococcal TSS encode certain SPEs (ie, A, C, F) capable of functioning as superantigens. These antigens induce a marked febrile response, induce proliferation of T lymphocytes, and induce synthesis and release of multiple cytokines, including tumor necrosis factor, interleukin-1 beta, and interleukin-6. This activity is attributed to the ability of the superantigen to simultaneously bind to the V-beta region of the T-cell receptor and to class II major histocompatibility antigens of antigen-presenting mononuclear cells, resulting in widespread, nonspecific T-cell proliferation and increased production of interleukin-2.
Nucleases
Four antigenically distinct nucleases (A, B, C, D) assist in the liquefaction of pus and help to generate substrate for growth.
Other products
Other extracellular products include NADase (leukotoxic), hyaluronidase (which digests host connective tissue, hyaluronic acid, and the organism’s own capsule), streptokinases (proteolytic), and streptodornase A-D (deoxyribonuclease activity).
[13]
Proteinase, amylase, and esterase are additional streptococcal virulence factors, although the role of these proteins in pathogenesis is not fully understood.
Suppurative disease spectrum
Streptococcal pharyngitis
S pyogenes causes up to 15-30% of cases of acute pharyngitis.
[14] Frank disease occurs based on the degree of bacterial virulence after colonization of the upper respiratory tract. Accurate diagnosis is essential for appropriate antibiotic selection.
Impetigo
Pyoderma is the most common form of skin infection caused by GAS. Also referred to as streptococcal impetigo or impetigo contagiosa, it occurs most commonly in tropical climates but can be highly prevalent in northern climates as well, particularly in the summer months. Risk factors that predispose to this infection include low socioeconomic status; low level of overall hygiene; and local injury to skin caused by insect bites, scabies, atopic dermatitis, and minor trauma. Colonization of unbroken skin precedes the development of pyoderma by approximately 10 days.
Streptococcal pyoderma may occur in children belonging to certain population groups and in overcrowded institutions. The modes of transmission are direct contact, environmental contamination, and houseflies. The strains of streptococci that cause pyoderma differ from those that cause exudative tonsillitis.
The bacterial toxins cause proteolysis of epidermal and subepidermal layers, allowing the bacteria to spread quickly along the skin layers and thereby cause blisters or purulent lesions. The other common cause of impetigo is Staphylococcus aureus.
Pneumonia
Invasive GAS can cause pulmonary infection, often with rapid progression to necrotizing pneumonia.
Necrotizing fasciitis
Necrotizing fasciitis is caused by bacterial invasion into the subcutaneous tissue, with subsequent spread through superficial and deep fascial planes. The spread of GAS is aided by bacterial toxins and enzymes (eg, lipase, hyaluronidase, collagenase, streptokinase), interactions among organisms (synergistic infections), local tissue factors (eg, decreased blood and oxygen supply), and general host factors (eg, immunocompromised state, chronic illness, surgery).
As the infection spreads deep along the fascial planes, vascular occlusion, tissue ischemia, and necrosis occur.
[15] Although GAS is often isolated in cases of necrotizing fasciitis, this disease state is frequently polymicrobial.
Otitis media and sinusitis
These are common suppurative complications of streptococcal tonsillopharyngitis. They are caused by the spread of organisms via the eustachian tube (otitis media) or by direct spread to the sinuses (sinusitis).
Nonsuppurative disease spectrum
Acute rheumatic fever
ARF is a delayed, nonsuppurative sequela of GAS tonsillopharyngitis. Following the pharyngitis, a latent period of 2-3 weeks passes before the signs or symptoms of ARF appear. The disease presents with various clinical manifestations, including arthritis, carditis, chorea, subcutaneous nodules, and erythema marginatum.
Rheumatic fever may be the result of host genetic predisposition. The disease gene may be transmitted either in an autosomal-dominant fashion or in an autosomal-recessive fashion, with limited penetrance. However, the disease gene has not yet been identified.
Considerable evidence supports the link between group A streptococcal infections of the upper respiratory tract and ARF, although only certain M-group serotypes (ie, 1, 3, 5, 6, 18, 24) are associated with this complication. Very mucoid strains, particularly strains of M type 18, have appeared in numerous communities prior to the appearance of rheumatic fever. Rheumatic fever is most frequently observed in children aged 5-15 years (the age group most susceptible to GAS infections).
The attack rate following upper respiratory tract infection is approximately 3% for individuals with untreated or inadequately treated infection. The latent period between the GAS infection and the onset of rheumatic fever varies from 2-4 weeks. In contrast to poststreptococcal glomerulonephritis (PSGN), which may follow either pharyngitis or streptococcal pyoderma, rheumatic fever can occur only after an infection of the upper respiratory tract.
Despite the depth of knowledge that has been accumulated about the molecular microbiology of Streptococcus pyogenes, the pathogenesis of ARF remains unknown. A direct effect of a streptococcal extracellular toxin, in particular streptolysin O, may be responsible for the pathogenesis of ARF, according to some hypotheses. Observations that streptolysin O is cardiotoxic in animal models support this hypothesis, but linking this toxicity to the valvular damage observed in ARF has been difficult.
A more popular hypothesis is that an abnormal host immune response to some component of the group A Streptococcus is responsible. The M protein of GAS shares certain amino acid sequences with some human tissues, and this has been proposed as a source of cross-reactivity between the organism and human host that could lead to an immunopathologic immune response. Also, antigenic similarity between the group-specific polysaccharide of S pyogenes and glycoproteins found in human and bovine cardiac valves has been recognized, and patients with ARF have prolonged persistence of these antibodies compared with controls with uncomplicated pharyngitis. Other GAS antigens appear to cross-react with cardiac sarcolemma membranes.
[16]
During the course of the host’s immune response to the GAS, the host’s antigens may, as a result of this molecular mimicry, be mistaken as foreign; this leads to an inflammatory cascade with resultant tissue damage. In patients with ARF with Sydenham chorea, common antibodies to antigens found in the S pyogenes cell membrane and the caudate nucleus of the brain are present, further supporting the concept of an aberrant autoimmune response in the development of ARF.
Interest in whether such autoimmune responses play a role in the pathogenesis of the syndrome known as pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) has been considerable, although further work is necessary to establish the link between streptococcal infections and these syndromes.
Poststreptococcal glomerulonephritis
Glomerulonephritis can follow group A streptococcal infections of either the pharynx or the skin, and incidence varies with the prevalence of so-called nephritogenic strains of group A streptococci in the community. Type 12 is the most frequent M serotype that causes PSGN after pharyngitis, and M type 49 is the serotype most commonly related to pyoderma-associated nephritis. The latent period between GAS infection and the onset of glomerulonephritis varies from 1-2 weeks.
Pathogenesis appears to be immunologically mediated. Immunoglobulins, complement components, and antigens that react with streptococcal antisera are present in the glomerulus early in the course of the disease, and antibodies elicited by nephritogenic streptococci are postulated to react with renal tissue in such a way as to promote glomerular injury. In contrast to acute rheumatic fever, recurrences of PSGN are rare. Diagnosis of PSGN is based on clinical history, physical examination findings, and confirmatory evidence of recent streptococcal infection.
Toxic shock syndrome
Severe GAS infections associated with shock and organ failure have been reported with increasing frequency, predominantly in North America and Europe.
Considerable overlap occurs between streptococcal TSS and streptococcal necrotizing fasciitis, insofar as most cases occur in association with soft-tissue infections. However, streptococcal TSS may also occur in association with other focal streptococcal infections, including pharyngeal infection.
The pathogenesis of streptococcal TSS appears to be related in part to the ability of certain (ie, A, C, F) streptococcal pyogenic exotoxins (SPEs) to function as superantigens.
Scarlet fever
When a fine, diffuse, erythematous rash is present in the setting of acute streptococcal pharyngitis, the illness is called scarlet fever. The rash of scarlet fever is caused by the pyrogenic exotoxins (ie, SPE A, B, C, and F). The rash highly depends on toxin expression; preexisting humoral immunity to the specific SPE toxin prevents the clinical manifestations of scarlet fever.
Scarlet fever has apparently become less common and less virulent than in past decades; however, incidence is cyclic, depending on the prevalence of toxin-producing strains and the immune status of the population. Modes of transmission, age distribution of cases, and other epidemiologic features are similar to those for streptococcal pharyngitis.
Central nervous system diseases
The primary evidence for poststreptococcal autoimmune central nervous system (CNS) disease is provided by studies of Sydenham chorea, the neurologic manifestation of rheumatic fever. Reports of obsessive-compulsive disorder (OCD), tic disorders, and other neuropsychiatric symptoms occurring in association with group A beta-hemolytic streptococcal infections suggest that various CNS sequelae may be triggered by poststreptococcal autoimmunity.
[17]






