Pulmonary Function Testing: Spirometry, Lung Volume Determination, Diffusing Capacity of Lung for Carbon Monoxide
Mục Lục
Description
Spirometry assesses the integrated mechanical function of the lung, chest wall, respiratory muscles, and airways by measuring the total volume of air exhaled from a full lung (total lung capacity [TLC]) to maximal expiration (residual volume [RV]). This volume, the forced vital capacity (FVC) and the forced expiratory volume in the first second of the forceful exhalation (FEV1), should be repeatable to within 0.15 L upon repeat efforts in the same measurement unless the largest value for either parameter is less than 1 L. In this case, the expected repeatability is to within 0.1 L of the largest value. The patient is instructed to inhale as much as possible and then exhale rapidly and forcefully for as long as flow can be maintained. The patient should exhale until one of the criteria defining the end of a forced exhalation has been reached. At the end of the forced exhalation, the patient should again inhale fully as rapidly as possible. The FVC should then be compared with that inhaled volume to verify that the forced expiratory maneuver did start from full inflation.
Reduction in FEV1 may reflect reduction in the maximum inflation of the lungs (TLC); obstruction of the airways; respiratory muscle weakness; or submaximal expiratory force due to poor coaching, poor understanding, or malingering. Airway obstruction is the most common cause of reduction in FEV1. Airway obstruction may be secondary to bronchospasm, airway inflammation, loss of lung elastic recoil, increased secretions in the airway, or any combination of these causes. Response of FEV1 to inhaled bronchodilators is used to assess the reversibility of airway obstruction, although it is now widely appreciated that a response showing a lack of a significant increase in FEV1 does not indicate the patient will not benefit clinically from bronchodilator therapy. A significant increase in the inspiratory capacity (IC) and/or vital capacity (VC) after bronchodilator therapy can occur even when the FEV1 fails to show a significant change.
[1]
The standards used to describe the quality of spirometry measurements are from the Standardization of Spirometry 2019 Update.
[2] This document provides examples of the most common technical problems associated with spirometry testing. See Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement for more information.
Indications
Spirometry is used to establish baseline lung function, evaluate dyspnea, detect pulmonary disease, monitor effects of therapies used to treat respiratory disease, evaluate respiratory impairment or disability, evaluate operative risk, and perform surveillance for occupational-related lung disease. It may also be used in research and clinical trials and epidemiological surveys.
Contraindications
Relative contraindications (no absolute contraindications) for spirometry are as follows:
-
Conditions that may be negatively impacted by the increases in myocardial demand or changes in blood pressure associated with spirometry: These include recent (< 1 week) myocardial infarction, systemic hypotension or severe hypertension, significant atrial/ventricular arrhythmia, noncompensated heart failure, uncontrolled pulmonary hypertension, acute cor pulmonale, clinically unstable pulmonary embolism, and a history of syncope associated with forced exhalation.
-
Conditions that may be negatively impacted by the increase in intracranial/intraocular pressure associated with spirometry: These include cerebral aneurysm, recent (< 4 weeks) brain surgery, recent concussion with continuing symptoms, and recent (within 1 week) eye surgery.
-
Conditions that may be negatively impacted by increased sinus and middle ear pressures: Examples include recent (< 1 week) sinus or middle ear surgery or infections.
-
Conditions that may be negatively impacted by increased intrathoracic and intraabdominal pressures: Examples include the presence of pneumothorax, recent (< 4 weeks) thoracic or abdominal surgery, and late-term pregnancy.
-
Infection control issues, including active or suspected transmissible respiratory or systemic infections including tuberculosis, or physical conditions predisposing to transmission of infections such as hemoptysis, significant secretions or oral lesions or bleeding
Patient care/preparations
Two choices are available with respect to bronchodilator and medication use prior to testing. Patients may withhold oral and inhaled bronchodilators to establish baseline lung function and evaluate maximum bronchodilator response, or they may continue taking medication as prescribed. If medications are withheld, a risk of exacerbation of bronchial spasm exists.
Interpretation
Interpretation of spirometry results should begin with an assessment of test quality. Failure to meet performance standards can result in unreliable test results (see the image below). The American Thoracic Society (ATS) defines acceptable spirometry as an expiratory effort that has the following characteristics:
Pulmonary function tests require patients to successfully perform respiratory maneuvers in a standardized manner in order to obtain clinically meaningful results. Spirometry is perhaps the most technically and physically demanding. The patient is required to inhale as fully as possible, exhale with as much force as possible, and continue their expiratory effort until they empty their lungs as completely as possible or are unable to continue.
The performance standards for acceptable spirometry are summarized below. The comments of the technologist administering the test can assist the interpreting physician in determining if results of a testing session that fail to meet some of the standards can still provide clinically useful data.
Table 1. Summary of Acceptability, Usability, and Repeatability Criteria for FEV1 and FVC (Open Table in a new window)
Acceptability and Usability
Required for Acceptability
Required for Usability
Criterion
FEV 1
FVC
FEV 1
FVC
Must have back extrapolated volume ≤5% of FVC or 0.100 L, whichever is greater
+
+
+
+
Must have no evidence of a faulty zero-flow setting
+
+
+
+
Must have no cough in the first second of expirationa
+
–
+
–
Must have no glottis closure in the first second of expirationa
+
+
+
+
Must have no glottis closure after 1 s of expiration
–
+
–
–
Must achieve one of these three end of forced expiration indicators:
-
Expiratory plateau (≤0.025 L in the last 1 s of expiration)
-
Expiratory time ≥15 s
-
FVC is within the repeatability tolerance of, or is greater than, the largest prior observed FVC
b
–
+
–
–
Must have no evidence of obstructed mouthpiece or spirometer
+
+
–
–
Must have no evidence of a leak
+
+
–
–
If the maximal inspiration following end of forced expiration is >FVC, then FIVC – FVC must be ≤ 0.100 L or 5% of FVC, whichever is greaterc
+
+
–
–
Repeatability Criteria (applied to acceptable FVC and FEV1 values)
Age >6 y: Difference between two largest FVC values must be ≤0.150 L, and the difference between two largest FEV1 values must be ≤0.150 L
Age ≤6 y: Difference between two largest FVC values must be ≤0.100 L or 10% of the highest value, whichever is greater, and the difference between two largest FEV1 values must be ≤0.100 L or 10% of the highest value, whichever is greater
aFor children ≤6 y, must have at least 0.75 s of expiration without glottis closure or cough for acceptable or useable measurement of FEV0.75.
bOccurs when the patient cannot expire long enough to achieve a plateau (eg, children with high elastic recoil or patients with restrictive lung disease) or the patient inspires or comes off the mouthpiece before a plateau. For within-maneuver acceptability, the FVC must be larger than or within the repeatability tolerance of the largest FVC observed before this maneuver within the current prebronchodilator or the current postbronchodilator testing set.
cAlthough the performance of a maximal forced inspiration is strongly recommended, its absence does not preclude a maneuver from being judged acceptable, unless extrathoracic obstruction is specifically being investigated.
Table 2. Quality Categories for FVC or FEV1 in Adults and Children (Open Table in a new window)
Grade
Criteria for Adults, Older Children, and Children Aged 2-6 Years
A
> 3 acceptable efforts with repeatability within 0.150 L
for age 2-6 y, 0.100 L, or 10% of highest value, whichever is greater
B
2 acceptable efforts with repeatability within 0.150 L
for age 2-6 y, 0.100 L, or 10% of highest value, whichever is greater
C
> 2 acceptable efforts with repeatability within 0.200 L
for age 2-6 y, 0.150 L, or 10% of highest value, whichever is greater
D
> 2 acceptable efforts with repeatability within 0.250 L
for age 2-6 y, 0.200 L, or 10% of highest value, whichever is greater
E
One acceptable effort
F
No acceptable efforts
Note that FEV1 and FVC each are graded separately.
Characteristics of acceptable spirometry efforts are as follows:
-
The patient is vigorously coached to inspire rapidly to full inflation.
-
The patient shows minimal hesitation at the start of the forced expiration (extrapolated volume < 5% of FVC or 0.10 L, whichever is larger).
-
The patients shows an explosive start of the forced exhalation (rise time to peak flow no greater than 0.150 s). Rise time to peak flow is not available on all spirometers. If it not available, it is not part of the assessment of the acceptability of the start of the forced exhalation.
-
The patient shows no evidence of cough or artifact in the first second of forced exhalation.
-
The results meets one of three criteria that define a valid end-of-forced exhalation: (1) smooth curvilinear rise of the volume-time tracing to a plateau (plateau defined as < 0.025 L volume change in the last 1 s of expiration) of at least 1 second’s duration; (2) if a forced test fails to exhibit an expiratory plateau, a forced expiratory time of 15 seconds; or (3) the FVC is within the repeatability tolerance of or is greater than the largest prior observed FVC.
-
Upon completing the forced exhalation, the patient is coached to rapidly (> 2 L/s flow) inhale to full inflation upon completing the forced exhalation providing a value for forced inspiratory vital capacity (FIVC). The maximum FIVC can be no more than 0.100 L or 5% of the FVC larger than the FVC (whichever is greater). If the maximum FIVC is more than 0.100 L or 5% of the FVC larger than the FVC, that effort is not acceptable and cannot be used for reporting of any parameters.
-
Repeatability of the largest FVC and FEV
1 within 0.150 L (within 0.100 L if age < 6 y) is demonstrated in at least two efforts.
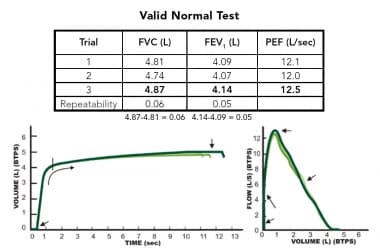
Example of an acceptable spirometry testing session showing evidence 3 efforts that show evidence of an explosive start of forced exhalation that continues until empty and good repeatability of forced vital capacity (FVC) and forced expiratory volume in the first second of the forceful exhalation (FEV1), which usually indicates all efforts started from full inflation.
View Media Gallery
Comprehensive treatment of technical acceptability of spirometry test results is beyond the scope of this review. Readers are directed to Spirometry Quality Assurance: Common Errors and Their Impact on Test Results. A booklet can also be obtained from the Department of Health and Human Services. It provides examples of common spirometry performance errors and their impact on test results.
In patients that have significant loss of lung elastic recoil (pulmonary emphysema, COPD), spirometry may show negative effort dependence of forced expiratory flow. The effort that has the highest peak expiratory effort may produce a lower FEV1 because of the dynamic compression of the airways that results from the loss of elastic recoil support of airways that is characteristic of emphysema. In this circumstance, reporting the highest FEV1 coming from an effort with submaximal expiratory effort can lead to confusing results, particularly if a setting of assessing spirometric response to bronchodilators. Although not yet a spirometry acceptability standard, it appears that when reporting the FEV1 considering only efforts that have a time to peak flow (TPEF) less than or equal to 0.12 seconds helps eliminate this effect. This parameter can be displayed on most laboratory-based spirometry testing systems.
Inspection of the volume-time tracing aids in identification of early termination of expiration by evaluating the presence of an expiratory plateau. In the absence of an expiratory plateau, a 15-second expiratory time ensures the quality of the FVC. Inspection of the start of the volume-time tracing can help identify a hesitant start, which can result in a falsely low FEV1. Repeatability of the FVC and the FEV1 helps ensure that the results truly represent the patient’s lung function. Attention should be focused on the repeatability of two key parameters: FVC and FEV1. It should be noted that while repeatability of the FVC and FEV1 strengthens the confidence that the forced exhalations started from full inflation, it is possible to demonstrate repeatability of these parameters even when forced exhalations start from a lung volume below full inflation. Demonstration that the difference between the largest FIVC and the FVC is no more than the larger of 0.100 L or 5% of the largest FIVC is a key acceptability criterion.
The reference equations published in 2012 by the Global Lung Initiative (GLI), a Task Force of the European Respiratory Society, provide normative values for males and females from age 3 to 95 years across a wide range of ethnicities,
[3] and these should be used as the default set of reference values for spirometry. The use of these predicted values for spirometry has been supported globally, including endorsements from the European Respiratory Society, the ATS, the American College of Chest Physicians, the Thoracic Society of Australia and New Zealand, the Australian and New Zealand Society of Respiratory Science, and the Asian Pacific Society for Respirology. The report is in accordance with the previously published recommendations of the ATS that called for the elimination of a fixed percent of predicted cut point to determine normality and a fixed lower limit of normal of the FEV1/FVC ratio to identify airway obstruction, both of which have been shown to result in significant misclassification of spirometry results.
[2] Guidelines for a standardized report format have been published and should be the default report format. The use of Z scores to determine severity of spirometric abnormalities is encouraged.
Abnormalities can be classified by the physiologic patterns outlined below.
Obstructive defects
Disproportionate reduction in the FEV1 as compared with the FVC is reflected in the FEV1/FVC ratio and is the hallmark of obstructive lung diseases. This physiologic category of lung diseases includes but is not limited to asthma, acute and chronic bronchitis, emphysema, bronchiectasis, cystic fibrosis, and bronchiolitis. The forced expiratory flow at any given lung volume is reduced. The mechanism responsible for the reduction in airflow can be bronchial spasm, airway inflammation, increased intraluminal secretions, and/or reduction in parenchymal support of the airways due to loss of lung elastic recoil. Poor understanding and effort on the part of the patient is also a cause for reduced flows, and the diagnosis of airway obstruction should be limited to measurements composed of acceptable efforts demonstrating repeatability of FVC and FEV1.
The use of a fixed lower limit of normal for the FEV1/FVC ratio as proposed by the Global Initiative for Obstructive Lung Disease (GOLD) lacks a scientific basis and results in significant misclassification of patients at either end of the age spectrum. Young patients are classified as “normal” when airflow obstruction is present, and older patients are classified as showing obstruction when no airflow obstruction is present. The use of the GOLD threshold for identifying airway obstruction should be discouraged in clinical practice where or when computerized predicted values are available.
The recommended practice for identifying a spirometric abnormality is to use the predicted lower limit of normal for that individual based on the sex, age, height, and ethnicity. The GLI reference equations provide lower limits of normal for spirometric parameters.
Assessment of reversibility of airway obstruction
When airway obstruction is identified on spirometry, assessing response to inhaled bronchodilators is useful. The ATS has recommended that the threshold for significant response be demonstration of an increase of at least 12% and 0.2 L in either FVC (provided the expiratory time for both sessions agree within 10%) or FEV1 on a spirogram performed 10-15 minutes after inhalation of a therapeutic dose of a bronchodilating agent. New standards recommend the use of four inhalations (100 mcg each, 400 mcg total dose) of albuterol administered through a valved spacer device. When concern about tremor or heart rate exists, lower doses may be used. Response to an anticholinergic drug may be assessed 30 minutes after four inhalations (40 mcg each, 160 mcg total dose) of ipratropium bromide. Failure to respond to bronchodilator challenge does not preclude clinical benefit from bronchodilators. A positive response to the bronchodilators may correlate with response to steroid therapy.
Restrictive defects
Reduction in the FVC with a normal or elevated FEV1-to-FVC ratio should trigger further evaluation of total lung capacity (TLC) to rule out restrictive lung disease. Measuring the TLC and residual volume (RV) can confirm restriction suggested by spirometry (see Lung Volume Determination below). See the chart below.
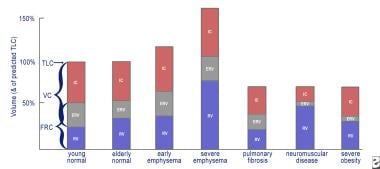
This is a graph of lung volumes in health and in disease, showing the various lung subdivisions. Normal aging results in an increase in functional reserve capacity (FRC) and residual volume (RV) and a normal total lung capacity (TLC) percentage. Obstructive lung diseases cause hyperinflation (increase in RV and FRC) with a relatively normal forced vital capacity (FVC). In severe emphysema, the TLC percentage can exceed 150%, with the RV impinging on the FVC. Restrictive lung diseases exhibit reduced TLC percentage with relative preservation of the RV/TLC percentage in fibrosis, a reduced inspiratory capacity and expiratory reserve volume (ERV) in neuromuscular disease, and severe reduction of the ERV in extreme obesity.
View Media Gallery
Quantification of impairment by spirometry
In normal spirometry, FVC, FEV1, and FEV1 -to-FVC ratio are above the lower limit of normal. The lower limit of normal is defined as the result of the mean predicted value (based on the patient’s sex, age, and height) minus 1.64 times the standard error of the estimate from the population study on which the reference equation is based. If the lower limit of normal is not available, the FVC and FEV1 should be greater than or equal to 80% of predicted, and the FEV1 -to-FVC ratio should be no more than 8-9 absolute percentage points below the predicted ratio. The ATS has recommended the use of lower limits of normal instead of the 80% of predicted for setting the threshold that defines abnormal test results.
A reduced FVC on spirometry in the absence of a reduced FEV1/FVC ratio suggests a restrictive ventilatory problem. An inappropriately shortened exhalation during spirometry can (and often does) result in an artifactually reduced FVC. Causes of restriction on spirometry include obesity, cardiomegaly, ascites, pregnancy, pleural effusion, pleural tumors, kyphoscoliosis, pulmonary fibrosis, neuromuscular disease, diaphragm weakness or paralysis, space-occupying lesions, lung resection, congestive heart failure, inadequate inspiration or expiration secondary to pain, and severe obstructive lung disease. One scheme for describing the severity of reductions in the FVC and/or the FEV1 is shown below:
-
Mild – Greater than 70% of predicted
-
Moderate – 60-69% of predicted
-
Moderately severe – 50-59%
-
Severe – 35-49% of predicted
-
Very severe – Less than 35% of predicted
The lower limit of normal for the FEF25-75% can be less than 50% of the mean predicted value, making it important to use the lower limit of normal defined by the 95% confidence limit of the mean predicted value rather than a threshold defined by a fixed percentage of the predicted value. The FEF25-75% is also very dependent on expiratory time. If expiratory times of spirometry efforts vary by more than 10%, comparisons of the FEF25-75% before and after bronchodilator challenge are difficult to interpret. Early termination of expiration shifts the middle 50% of the exhaled volume toward the start of the exhalation, artifactually raising the FEF25-75%. For these reasons, the use of the FEF25-75% to assess airway function in adults is discouraged.
The FVC is a reliable means of assessing the clinical status in idiopathic pulmonary fibrosis (IPF). A minimum clinically important difference of the FVC, expressed as a percentage of the mean predicted normal value, of 2-6% of has been established. This obviates the need to obtain a total lung capacity (TLC) measurement to assess disease progression or the effects of medical therapy.
Special assessments
Sitting versus supine vital capacity
Evaluation of diaphragm strength can be accomplished by measuring the vital capacity in an upright or sitting position followed by a measurement made in the supine position. A reduction in the vital capacity to less than 90% of the upright vital capacity suggests diaphragm weakness or paralysis. Interpreting an increased reduction in vital capacity in the supine position as diaphragm dysfunction should be made cautiously if the patient’s body mass index is greater than 45 kg/m2.
[4] Studies reporting the normal reduction of the vital capacity of less than 10% from upright to supine were conducted with individuals who were not obese. Slightly greater reductions in obese individuals in a supine position may not indicate diaphragm dysfunction, but rather an increase in the resistive forces against which the diaphragm descends. Reductions in the supine vital capacity more than 20% of baseline indicate hemidiaphragm or diaphragm dysfunction or paralysis.
Identifying central airway obstructions
The configuration of the flow-volume curve of a properly performed spirometry test can be used to demonstrate various abnormalities of the larger central airways (larynx, trachea, right and left mainstem bronchi). Three patterns of flow-volume abnormalities can be detected: (1) variable intrathoracic obstructions, (2) variable extrathoracic obstructions, and (3) fixed upper airway obstructions. Reproducing these findings on every effort is important because spurious nonreproducible reductions in inspiratory flow are not uncommon after completion of forced expirations in subjects without upper airway obstruction. Examples of variable intrathoracic obstruction include localized tumors of the lower trachea or mainstem bronchus, tracheomalacia, and airway changes associated with polychondritis.
Variable upper airway obstructions demonstrate flow reductions that vary with the phase of forced respirations. Variable intrathoracic obstructions demonstrate reduction of airflow during forced expirations with preservation of a normal inspiratory flow configuration. This is observed as a plateau across a broad volume range on the expired flow limb of the flow-volume curve. The reduction in airflow results from a narrowing of the airway inside the thorax, in part because of a narrowing or collapse of the airway secondary to extraluminal pressures exceeding intraluminal pressures during expiration.
Variable extrathoracic obstructions demonstrate reduction of inspired flows during forced inspirations with preservation of expiratory flows. Again, the major cause of the reduced flow during inspiration is airway narrowing secondary to extraluminal pressures exceeding intraluminal pressures during inspiration. Causes of this type of upper airway obstruction include unilateral and bilateral vocal cord paralysis, vocal cord adhesions, vocal cord constriction, laryngeal edema, and upper airway narrowing associated with obstructive sleep apnea.
Fixed upper airway obstructions demonstrate plateaus of flow during both forced inspiration and forced expiration. Causes of fixed upper airway obstruction include goiters, endotracheal neoplasms, stenosis of both main bronchi, postintubation stenosis, and performance of the test through a tracheostomy tube or other fixed orifice device. (See the image below.)
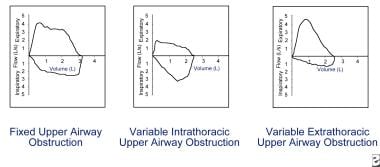
Flow reduction must be consistent on every effort to be considered actual flow limitation. Fixed upper airway obstruction may be caused by postintubation stenosis, goiter, endotracheal neoplasms, and bronchial stenosis. Variable intrathoracic obstruction may be caused by tracheomalacia, polychondritis, and tumors of the lower trachea or main bronchus. Variable extrathoracic obstruction may be caused by bilateral and unilateral vocal cord paralysis, vocal cord constriction, reduced pharyngeal cross-sectional area, and airway burns.
View Media Gallery
Assessment of operative risk
While no single test can effectively predict intraoperative and postoperative morbidity and mortality from pulmonary complications, the FEV1 obtained from good quality spirometry is a useful tool. When the FEV1 is greater than 2 L or 50% of predicted, major complications are rare.
Operative risk is heavily dependent on the surgical site, with chest surgery having the highest risk for postoperative complications, followed by upper and lower abdominal sites. Patient-related factors associated with increased operative risk for pulmonary complications include preexisting pulmonary disease, cardiovascular disease, pulmonary hypertension, dyspnea upon exertion, heavy smoking history, respiratory infection, cough (particularly productive cough), advanced age (>70 y), malnutrition, general debilitation, obesity, and prolonged surgery.
Assessment for lung surgery typically involves prediction of a postoperative FEV1 by using the preoperative FEV1. In a borderline case, consideration of the contribution of the remaining portions can be assessed by a perfusion scan. The relative percentage of perfusion (Q) of the remaining lung or lung segments usually is proportional to its contribution to ventilation and can be used to estimate postoperative function as shown in the following equation:
Postoperative FEV1 = Preoperative FEV1 × Q% of the remaining lung
For example, if the preoperative FEV1 is 1.6 L and the lung to be resected demonstrates 40% perfusion, the postoperative FEV1 would be 1.6 × 0.6 = 0.96 L. An estimated postoperative FEV1 of less than 0.8 L often is associated with chronic respiratory failure and may indicate an unacceptable degree of operative risk. Arterial blood gases (ABGs) and cardiopulmonary exercise testing may help evaluate operative risk in patients who have a preoperative FEV1 below 2 L or 50% of predicted.
The algorithm for clearance of candidates for lung resection proposed by Bolinger and Perruchoud
[5] has been successfully evaluated in 137 consecutive patients who were referred for resection by Wyser et al
[6] with an overall mortality of 1.5% and is detailed in Cardiopulmonary Stress Testing. Patients with a negative cardiac history and ECG that demonstrate an FEV1 and a diffusing capacity of lung for carbon monoxide (DLCO) that are greater than 80% of predicted are judged to be able to undergo pneumonectomy safely.
Technical considerations
The ATS has published guidelines for a standardized technique that includes spirometer performance standards. A reasonable end-point for the maneuver in the absence of true flow cessation (ie, airway obstruction is present) is 15 seconds. Patients often discontinue the forced exhalation prematurely because of the discomfort of prolonged forced exhalation. A modified technique in which the patient exhales with maximum force for four seconds followed by continued relaxed exhalation has been shown to enhance the patient’s ability to sustain expiration, thereby yielding a larger FVC in patients with airflow obstruction. It should be noted that, strictly speaking, the FVC obtained from using this technique is not a true FVC because maximum expiratory effort was not sustained during the entire exhalation.






